Ready to take the exciting leap into parenthood? Understanding your fertility cycle is a major first step.
If you’re on a mission to conceive, keeping a close eye on ovulation symptoms and scheduling intimate moments during your fertile window can significantly boost your chances.
Knowing when you’re ovulating is the golden ticket in your pregnancy journey. But we’re not just here to help you decode the signs of ovulation—we’re going to guide you through recognizing when the show’s over too.
Fortunately, there’s an array of ovulation symptoms that you can team up with ovulation tests or apps to help you detect ovulation. But knowing when you’re ovulating is only half the picture—it’s equally crucial to determine the signs ovulation is over.
Let’s explore the nine signs that ovulation is over to help you navigate your cycle from start to end.
Signs Ovulation Is Over
From observing the texture of your cervical mucus to shifts in your mood and sexual desire, here are nine indicators that suggest ovulation has ended.
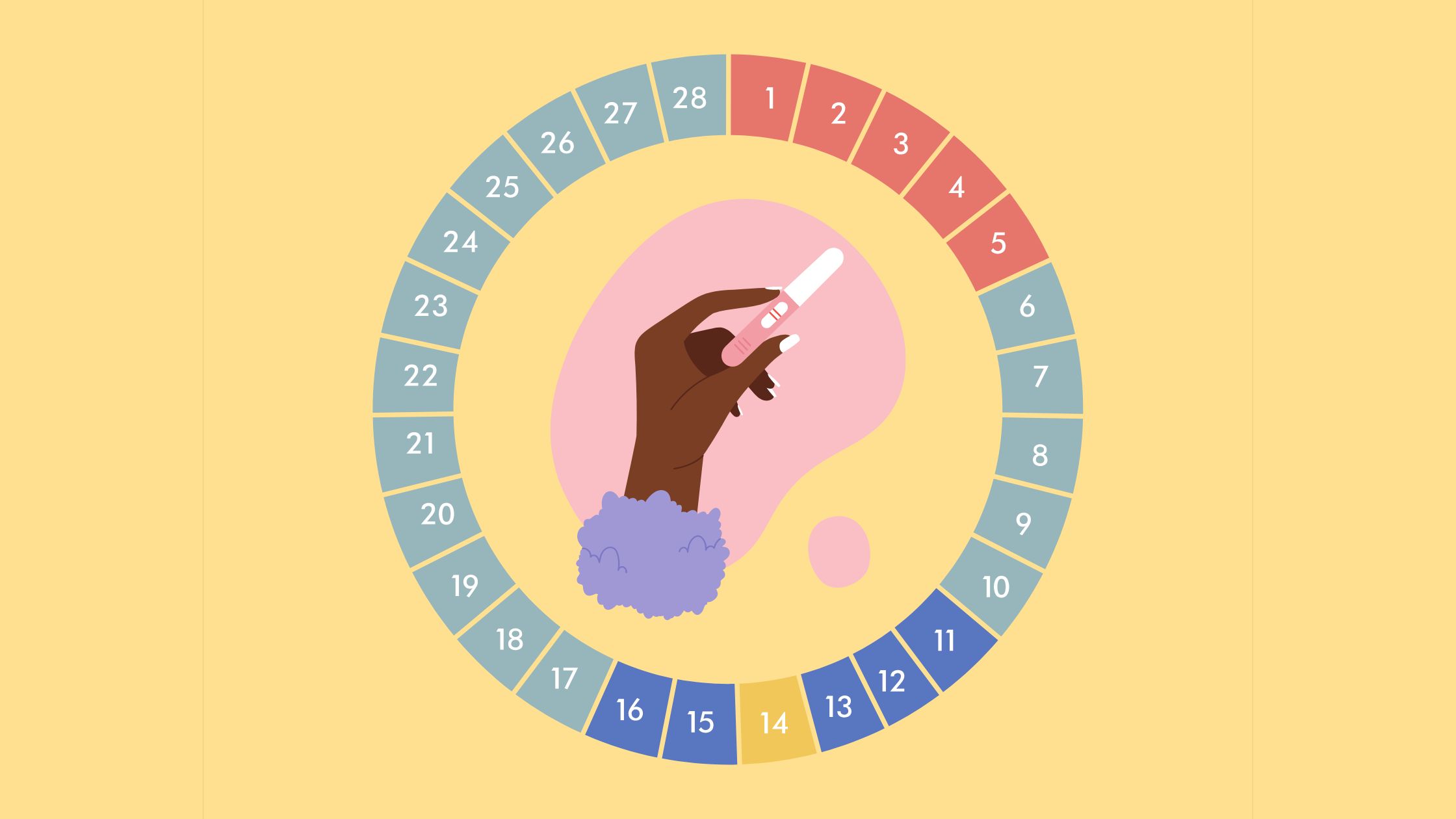
1. Calendar Confirms it
One of the most clear signs that ovulation has occurred is when the dates on your menstrual calendar align with your typical ovulatory period. As ovulation generally happens about two weeks prior to the onset of menstruation, keeping a precise record of your menstrual cycles is invaluable. Notably, in a typical 28-day cycle, ovulation occurs around day 14. However, individual cycle lengths may vary, making it essential to adjust predictions accordingly.
Using an ovulation calculator and calendar can help you predict ovulation dates. The only information required is the date of the first day of your last menstrual cycle and the average duration of your period.
2. Cervical Mucus Changes
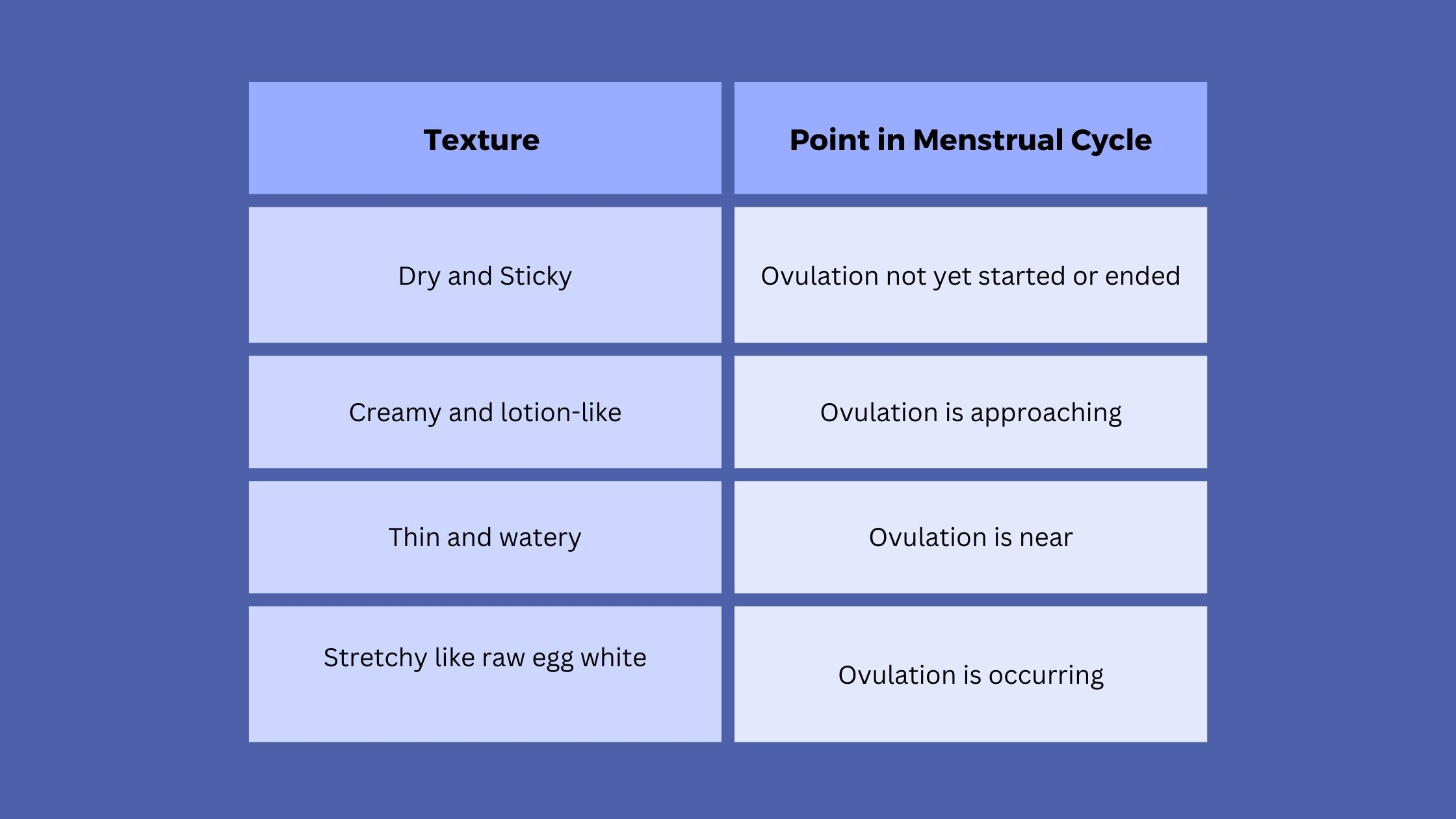
Cervical mucus plays a crucial role in a woman’s fertility cycle, providing valuable insights into ovulation and the overall menstrual cycle. Changes in its texture, color, and volume throughout the menstrual cycle are influenced by fluctuating hormone levels.
Before ovulation, the cervical mucus is typically thick, white, and dry. Its purpose at this stage is to prevent infection by blocking the passage to the cervix. The mucus at this stage is not very conducive to sperm movement.
During ovulation, which is a crucial event in the menstrual cycle and involves the release of a mature egg, cervical mucus undergoes significant changes. It increases in volume and becomes clear and slippery, resembling raw egg whites. This is one of the major signs of ovulation. These changes are primarily due to hormonal fluctuations, notably a rise in estrogen levels, and serve to facilitate the passage of sperm toward the egg. This type of mucus is indicative of the most fertile period for conception.
After ovulation, the hormone progesterone becomes dominant. This leads to changes in the cervical mucus, returning it to its pre-ovulation state, characterized by being creamy, sticky, and thick. These changes mark the end of the fertile window.
In early pregnancy, there may be an increase in mucus with a runny, watery texture. Implantation bleeding can also cause the mucus to have a pink tinge. However, it’s important to note that not all pregnant women experience noticeable changes in cervical fluid. Also, these changes may not be immediately apparent due to the time it takes for pregnancy hormones to build up in the body.
Nevertheless, tracking changes in cervical mucus can be beneficial for those trying to conceive and those using natural methods of birth control.
3. Lower and Firmer Cervical Position
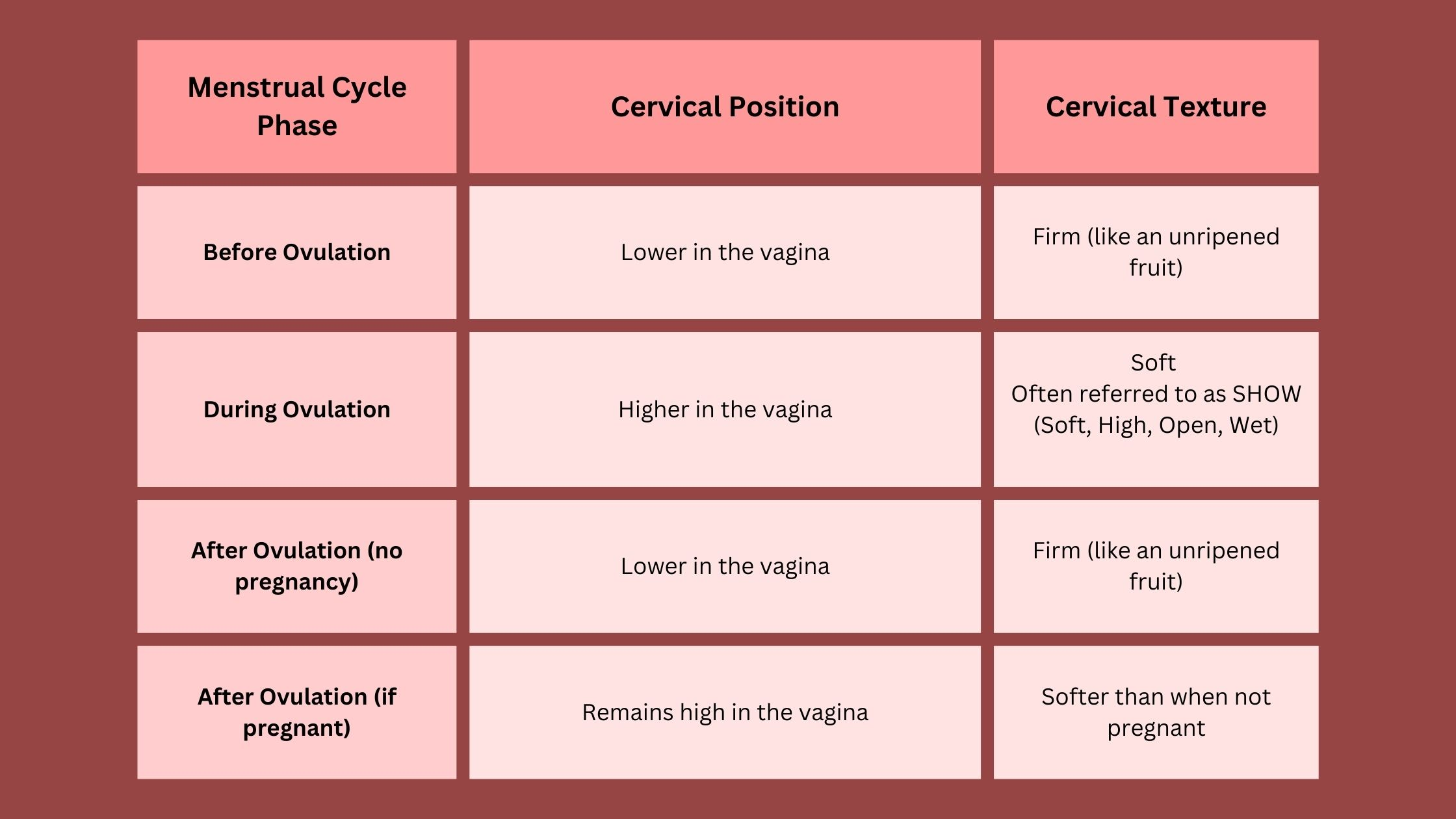
The cervix connects the vagina to the uterus. It changes position, texture, and texture throughout the menstrual cycle.
Before ovulation, the cervix is relatively lower in the vagina and feels firm, similar to an unripe fruit.
During ovulation, the cervix rises higher in the vagina, and its texture changes to become soft. This position and texture are often abbreviated to SHOW, meaning that the cervix is Soft, High, Open, and Wet.
After ovulation, if pregnancy hasn’t occurred, the cervix drops lower in the vagina and becomes firm, similar to its pre-ovulation state. However, if pregnancy has occurred, the cervix remains high in the vagina, similar to its position during ovulation.
These changes can provide valuable information for those trying to conceive or avoid pregnancy. It’s possible to check the position and firmness of the cervix at home. However, it requires practice and care.
While these are general patterns, individual differences can exist. Therefore, it is important to familiarize oneself with one’s own cervical patterns throughout the menstrual cycle for accurate interpretations.
4. Increase in Basal Body Temperature (BBT)
An increase in basal body temperature is one of the signs of ovulation.
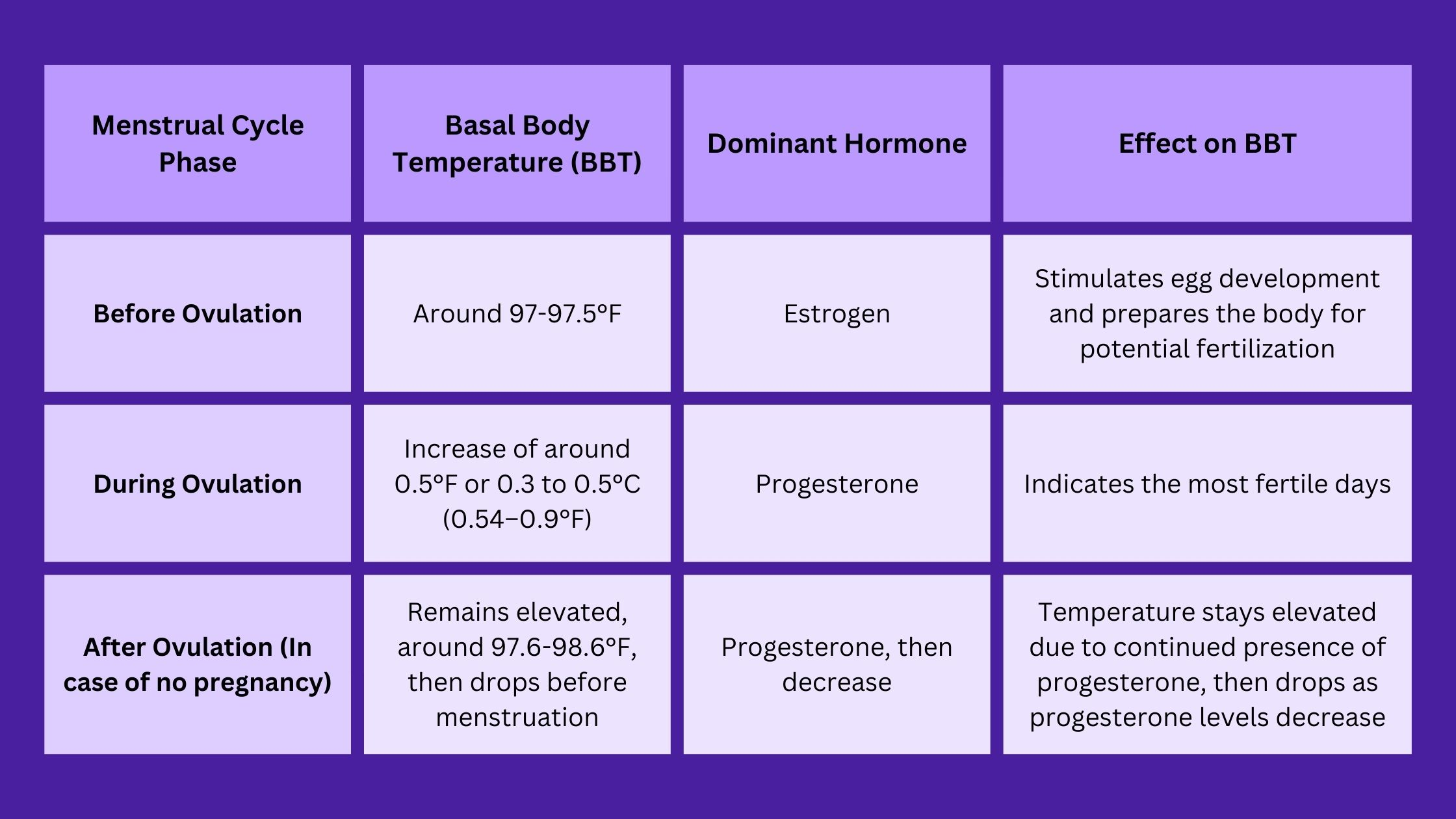
Basal body temperature refers to the body’s temperature at rest. Throughout the menstrual cycle, basal body temperature tracking can help confirm ovulation.
Before ovulation, basal body temperature averages around 97-97.5°F. The main hormone influencing this phase is estrogen, which stimulates egg development and prepares the body for potential fertilization.
During ovulation, the body experiences a slight increase in BBT. There is usually an increase of around half a degree Fahrenheit, or between 0.3 to 0.5 °C (0.54–0.9 °F). This temperature rise, resulting from the secretion of progesterone, indicates the most fertile days.
After ovulation, a woman’s body temperature stays a bit higher, usually between 97.6-98.6°F. This is because of a hormone called progesterone. If she doesn’t get pregnant, this temperature drops before her next period. But, if she does get pregnant, the temperature stays high.
These BBT fluctuations provide important information for fertility planning. However, the process of tracking BBT requires accuracy and consistency. It’s best to measure BBT in the morning before getting out of bed or engaging in any physical activity, as any movement can alter body temperature.
Moreover, various factors like stress, illness, lack of sleep, or alcohol consumption can affect BBT, so it’s important to note any potential influencing factors when charting BBT.
5. Decrease in Sexual Drive
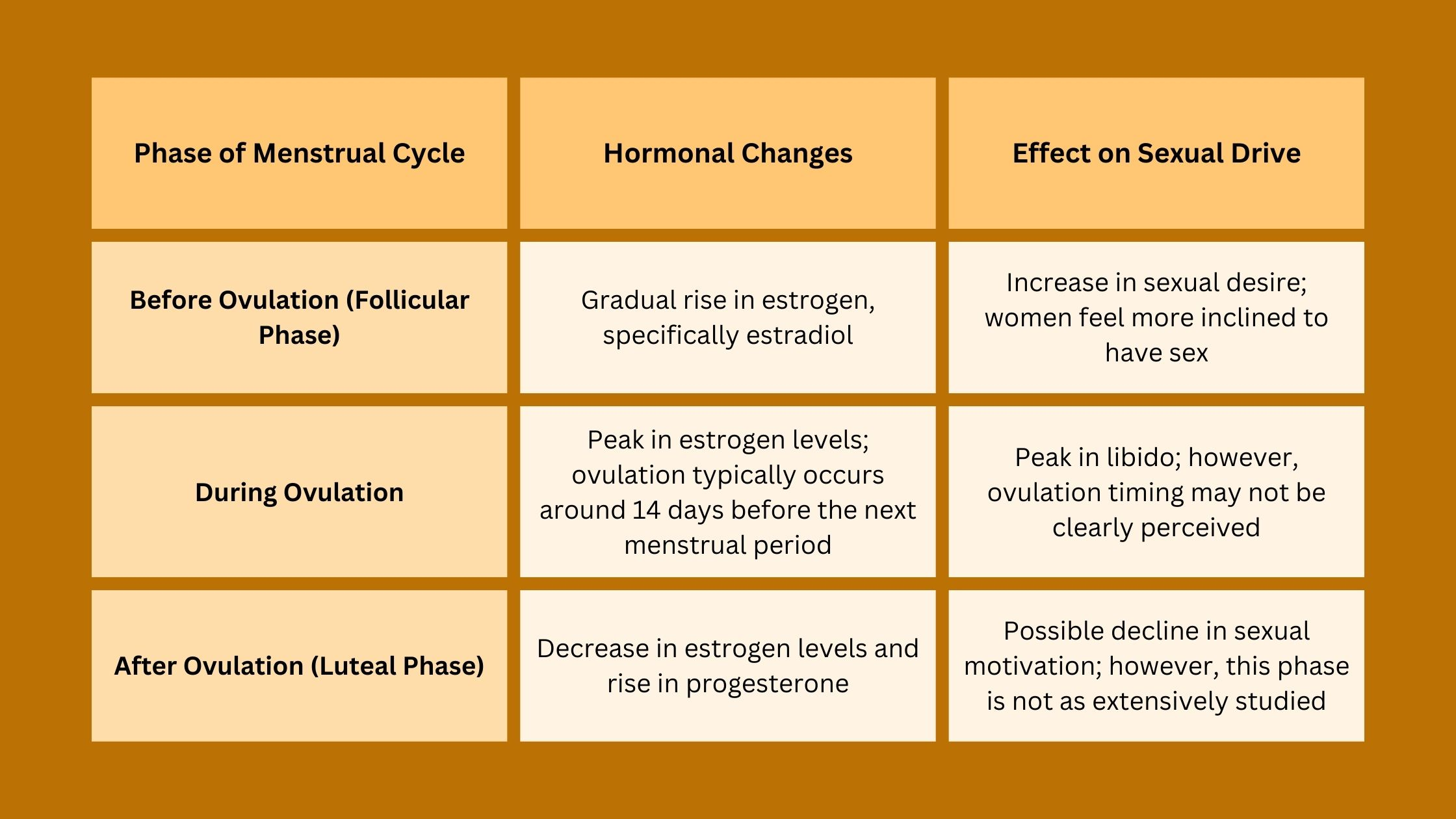
Sexual drive or libido can be influenced by various factors, one of which includes hormonal changes associated with the menstrual cycle. Studies suggest that the levels of sexual desire in women can fluctuate throughout different phases of the menstrual cycle, showing a cyclical pattern in correlation with hormonal changes.
Before ovulation, during the follicular phase of the menstrual cycle, estrogen levels gradually rise. This increase in estrogen, specifically estradiol, is linked to increased sexual desire, with women often feeling more inclined to have sex.
During ovulation, which typically occurs around 14 days before the next menstrual period, women experience a peak in libido. This peak in libido is likely due to evolutionary reasons where increased sexual interest could facilitate conception.
After ovulation, estrogen levels decrease, and progesterone becomes dominant. The impact of these hormonal changes on women’s sexual drive is not as extensively studied as the pre-ovulation and ovulation phases. But, it is reasonable to assume that there might be some decline in sexual motivation as the levels of estrogen, which is associated with increased libido, decrease.
During pregnancy, changes in hormone levels can also impact sexual drive. For example, increased sex drive is common during the early stages of pregnancy, particularly prevalent during the second trimester.
However, it’s important to note that the effects can vary among individuals, with some experiencing a strong desire for sex while others may have a decreased interest, potentially due to discomforts such as nausea and vomiting.
6. Breasts Become Tender
Once ovulation takes place, the luteal phase of the menstrual cycle follows. This phase often comes with symptoms like:
- nausea
- headaches
- fatigue
- muscle aches
- breast tenderness
The symptoms generally begin post-ovulation and may persist until the start of the next menstrual cycle.
As estrogen levels decline and progesterone levels rise after ovulation, the breasts may become more sensitive or swollen. Hence, any mid-cycle change in breast tenderness could signal that ovulation has occurred.
7. Relief from Abdominal Cramps
Abdominal cramps can be an ovulation symptom. This lower abdominal pain, also known as mittelschmerz, is usually a dull, achy sensation on one side of the lower abdomen but can be sharp for some women.
While the pain typically lasts for a short duration, usually before and during ovulation, it can sometimes persist after ovulation. Post-ovulation cramping can be normal and might indicate the start of the luteal phase of the menstrual cycle. But it can also be linked to other conditions such as ovarian cysts, endometriosis, or pelvic congestion syndrome.
The intensity of post-ovulation pain varies, and it can occur with spotting. The cramps may last for a day to a week after ovulation, and their meaning changes as time progresses. In some cases, post-ovulation cramping could potentially indicate implantation, signifying the early stages of pregnancy.
However, the occurrence of cramps, including their timing and intensity, can vary greatly among women and from cycle to cycle. Some women may experience cramping with every cycle, while others might only experience it occasionally or not at all.
Therefore, while post-ovulation cramps can sometimes suggest that ovulation has taken place, they are not definitive sign that ovulation has ended.
8. Changes in Mood
The menstrual cycle, which typically lasts for around 28 days, involves a series of hormonal changes that can influence mood and behavior.
Before ovulation (Follicular phase): Rising estrogen levels can improve mood and energy, enhancing socialization, motivation, and cognitive abilities.
During ovulation (Ovulatory phase): A peak in estrogen can lead to mood variations, ranging from irritability to increased energy and even heightened libido. However, the dip in estrogen that follows ovulation can cause mood swings, irritability, anger, and in some cases, short-lived depression.
After ovulation (Luteal phase): Some women may experience mood swings, irritability, or feelings of sadness in the days following ovulation, often referred to as premenstrual syndrome (PMS). In severe cases, these can escalate to premenstrual dysphoric disorder (PMDD), significantly impacting daily life.
While these patterns are generally observable, individual experiences can vary greatly due to factors such as stress, sleep quality, illness, and life events. Hormonal contraceptives can also influence mood changes.
9. Use an Ovulation Predictor Kit
Still can’t tell when your ovulation occurs? Ovulation predictor kits are a handy tool for tracking ovulation to help identify the luteinizing hormone (LH) surge typically occurring one to two days before ovulation. However, their utility extends beyond predicting ovulation. A negative result following a positive one can indicate ovulation has likely concluded, providing tangible confirmation to corroborate other symptoms.
Takeaway
- By identifying ovulation signs, you may be able to tell whether or not you are ovulating.
- The menstrual calendar can confirm if ovulation has occurred if the dates align with the typical ovulatory period.
- After ovulation, cervical mucus returns to a creamy, sticky, and thick state, indicating the end of the fertile window.
- After ovulation, if pregnancy hasn’t occurred, the cervix drops lower and becomes firm again, returning to its pre-ovulation state.
- Basal body temperature remains elevated after ovulation due to the presence of progesterone and falls before the next menstrual cycle starts.
- It’s believed that there might be some decline in sexual drive as the levels of estrogen decrease.
- The completion of ovulation can lead to symptoms such as nausea, headaches, fatigue, muscle aches, and continued breast tenderness, indicating the start of the luteal phase of the menstrual cycle.
- The end of mittelschmerz (abdominal cramps indicating ovulation) could signal the end of ovulation, but other conditions can cause similar symptoms, so consultation with a doctor is advisable.
- Hormonal fluctuations after ovulation can lead to premenstrual syndrome (PMS) symptoms, including irritability, anxiety, and depression.
- A negative result on an ovulation predictor kit after a positive one can suggest that the ovulation phase has concluded.
References
Cleveland Clinic. (n.d.). Cervical Mucus. Retrieved July 20, 2023, from https://my.clevelandclinic.org/health/body/21957-cervical-mucusUniversity of Michigan Health. (n.d.). Cervical Mucus: Frequently Asked Questions. Retrieved July 20, 2023, from https://www.uofmhealth.org/health-library/hw202058Castleman, M. (2015, March 26). How the menstrual cycle affects women's libido. Psychology Today. https://www.psychologytoday.com/us/blog/all-about-sex/201503/how-the-menstrual-cycle-affects-womens-libidoRoney, J. R., & Simmons, Z. L. (2013, Feb, 20). The evolutionary psychology of human mate choice: How ecology, genes, fertility, and fashion influence mating behavior. https://labs.psych.ucsb.edu/roney/james/roneysimmons.published.pdfShackelford, T. (2018, March 1). Sex Cycle. Psychology Today. https://www.psychologytoday.com/us/blog/how-we-do-it/201803/sex-cycleCleveland Clinic. (n.d.). Ovulation Pain (Mittelschmerz). Retrieved July 20, 2023, from https://my.clevelandclinic.org/health/diseases/9134-ovulation-pain-mittelschmerzBull, J. R., Rowland, S. P., Scherwitzl, E. B., Scherwitzl, R., Danielsson, K. G., & Harper, J. (2019). Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. Npj Digital Medicine, 2(1), 1-8. doi.org/10.1038/s41746-019-0152-7Smith, S. (n.d.). Does Ovulation Cause Depression? Experts Explain. Romper. Retrieved July 20, 2023, from https://www.romper.com/pregnancy/does-ovulation-cause-depression-experts-explainCleveland Clinic. (n.d.). Premenstrual Dysphoric Disorder (PMDD). Retrieved July 20, 2023, from https://my.clevelandclinic.org/health/articles/9132-premenstrual-dysphoric-disorder-pmdd